Colorectal Cancer: Your Questions Answered
6 min read
Cancers that form in your colon or rectum are collectively called colorectal cancer. Colorectal cancer is the fourth most common cancer in the United States, but the number of cases is in decline due to more screenings and better public awareness of the lifestyle changes people need to make to avoid it.
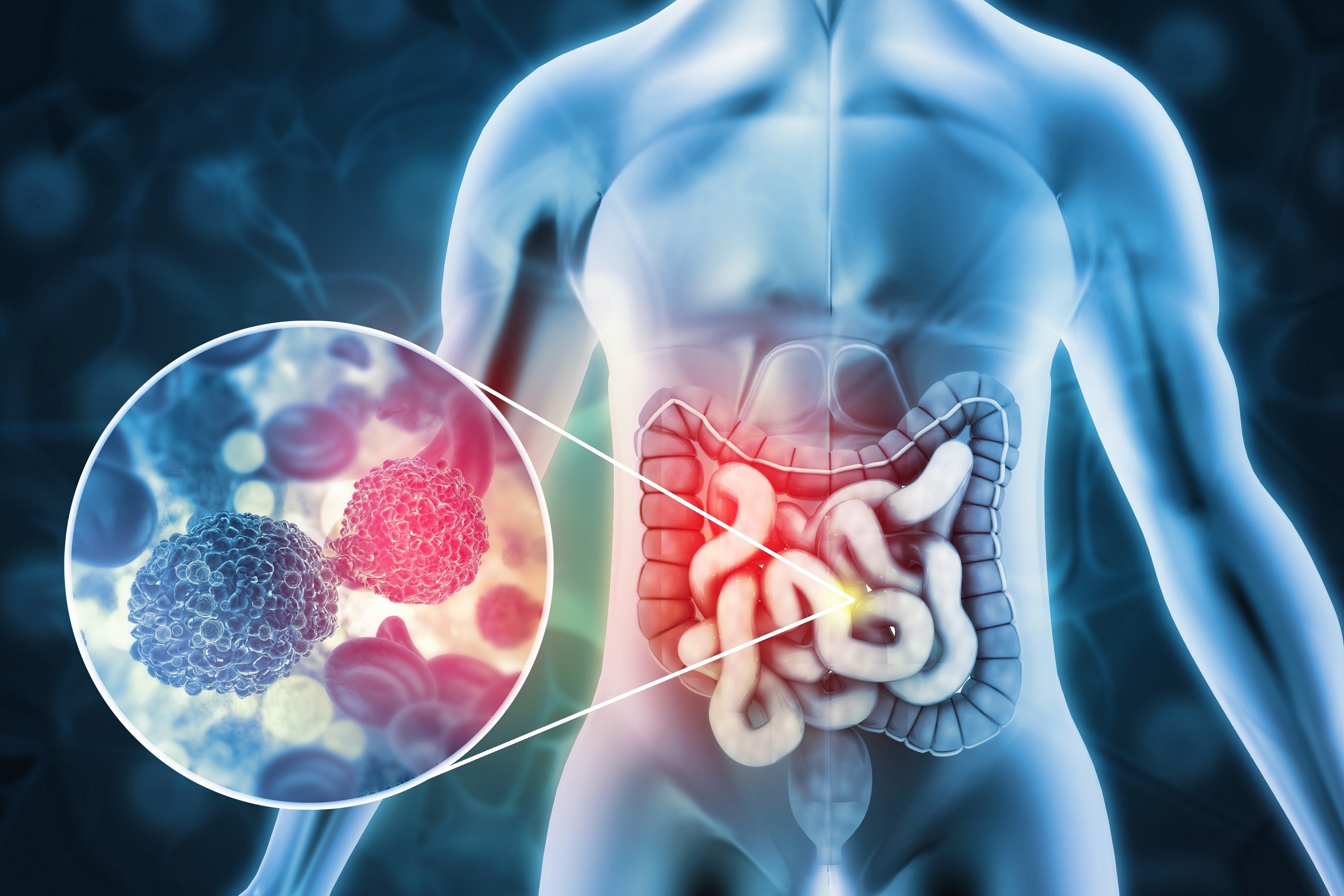
What Is Colorectal Cancer?
Colorectal cancer can form anywhere in your large intestine, which includes both your colon and rectum. The colon makes up a majority of the large intestine while the rectum makes up the last six inches. The type of cancer you’re diagnosed with is typically based on where it starts. For example, a colon cancer diagnosis means cancerous cells were first found in your colon.
According to the American Cancer Society, your average risk for developing colorectal cancer is 1 in 23 in men and 1 in 25 in women.
What Are Polyps?
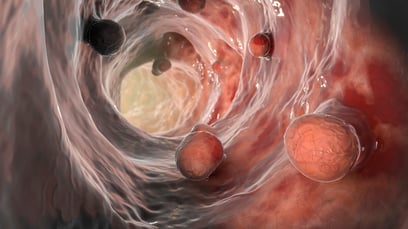 Polyps are growths on the lining of your colon. Not all polyps are cancerous, but they can become cancerous. Polyps can be large or small and may appear flat or raised. They sometimes look bumpy or have a stem. Colon polyps are often where colorectal cancers start. They’re one of the main things a physician is looking for during a colonoscopy for colorectal screening.
Polyps are growths on the lining of your colon. Not all polyps are cancerous, but they can become cancerous. Polyps can be large or small and may appear flat or raised. They sometimes look bumpy or have a stem. Colon polyps are often where colorectal cancers start. They’re one of the main things a physician is looking for during a colonoscopy for colorectal screening.
What Causes Colorectal Cancer?
Like all forms of cancer, colorectal cancer is caused when damaged cells begin to multiply too quickly. Scientists aren’t exactly sure what causes cells to grow like this, but they do know people are at increased risk if they have certain lifestyle habits or genetic markers, such as the presence of a gene for Lynch syndrome.
Learn more about colorectal cancer risk factors.
It does appear that lifestyle plays an important role in risk of developing colorectal cancer. What you eat can have an impact, over time, on the changes that occur in the colon. The added chemicals in processed foods and our overall dietary habits may be related to why more young people are developing colorectal cancer.
Read More: Colorectal Cancer is on the Rise in Younger People.
Are There Any Symptoms of Colorectal Cancer?
It’s rare for early-stage colorectal cancers to have any symptoms. This makes being screened for colorectal cancers important. Talk to your doctor if you notice any of the following symptoms:
- Blood in your stool
- Changing bowel habits or stool shape
- Dark or black stools
- Decreased appetite
- Long-lasting constipation or diarrhea
- Pain or cramping in the abdomen
- Rectal bleeding
- Unintended weight loss
- Urge to defecate when the bowel is already emptied
Read more about signs and symptoms of colorectal cancer.
Am I At Risk for Developing Colorectal Cancer?
You can’t change certain risk factors, such as genetics or age, but you can adjust lifestyle choices, such as diet and exercise. The risk factors you can’t control include:
- Being over age 50
- Gastrointestinal or autoimmune disease such as inflammatory bowel disease (IBD), ulcerative colitis, or Crohn’s disease
- Family history of colorectal cancer or cancerous polyps
- History of colon polyps
- Inherited gene mutations that can lead to cancer
- Race: African Americans and those of Ashkenazi descent have the highest rates of colorectal cancer
Meanwhile, lifestyle risk factors for colorectal cancer include:
- Being overweight or obese
- Type 2 diabetes
- Heavy alcohol consumption
- Lack of exercise
- Smoking or tobacco use
- Unhealthy diet that's high in processed foods and sugar
Read More: Ultra-Processed Foods and Their Connection to Colorectal Cancer
What Can I Do to Reduce My Risk of Developing Colorectal Cancer?
Approximately 75% of new colorectal cancer diagnoses occur in patients who have no identifiable risk factors. Despite this, there are several steps you can take to improve your overall health and reduce your colorectal cancer risk.
 Get screened for colon cancer.
Get screened for colon cancer.- Eat a healthy diet. A regular diet high in lean protein sources, fresh fruits, vegetables, and whole grains helps reduce cancer risk and maintain health. Reduce your consumption of red meat and processed foods such as lunch meats, prepared foods, and sugary drinks.
- Maintain a healthy weight. Preventing obesity is important for reducing your risk of colorectal cancer and other diseases such as type 2 diabetes and heart disease. Eating a healthy diet and staying active makes this easier.
- Reduce alcohol consumption. Moderate to severe alcohol consumption has shown to increase the risk of colorectal cancer. High risk individuals should stop drinking or reduce their consumption to two drinks a day for men and one for women.
- Stay active. Physical activity and exercise help reduce cancer risk and maintain a healthy weight. The American Heart Association recommends 150 minutes a week of moderate-intensity activity. This can include walking, gardening, dancing, riding a bike, or swimming.
- Stop smoking. There’s no part of your health that doesn’t benefit from quitting smoking. Stop smoking or using tobacco to reduce your cancer risk and stay healthy in the long term.
When Should I Be Screened for Colorectal Cancer?
Screening for colorectal cancer is one of the most effective ways to reduce your risk. Research indicates colonoscopies help find colorectal cancers early and decrease the likelihood that the disease will be fatal.
Screenings are recommended for average-risk Americans ages 45 and older. Colonoscopies are recommended every ten years for those at average risk while two-step screening methods are recommended annually. For adults with an increased risk, screenings may be recommended before age 45. If you’re over the age of 75, speak to your doctor for recommended screening schedules.
Get our complete guide to colorectal cancer screening.
There are several screening methods:
- Colonoscopy. A colonoscopy involves inserting a scope into the rectum to examine your colon. The procedure is typically performed under sedation and involves some preparation beforehand. The benefits of a colonoscopy are that a physician can identify and remove polyps and detect cancer in a single test.
- Imaging test. This involves using external machines to take an internal image of the colon and rectum. A colonoscopy is needed to confirm the presence of cancer, which is why it is referred to as a “two-step method.”
- Stool-based test. This method involves examining a stool sample for signs of potential cancer. This is also a two-step method that requires a colonoscopy to confirm a diagnosis.
Many people are reluctant to schedule their colorectal cancer screenings because of the preparation process. Colonoscopies are not painful and are performed under mild sedation. Most patients don’t even remember the procedure once it’s been completed. If you’re unsure about the process, talk to your doctor.
Learn more about at-home colorectal cancer screening tests.
Treatment for Colorectal Cancer
Treatment options for colorectal cancer depend on its stage, which is defined by how much the cancer has grown and how far it has spread. In the earlier stages, before the cancer spreads to lymph nodes near your colon, you may only need surgery. Depending on how likely the cancer might return, you may also need chemotherapy. In stage 3, when the cancer has spread to nearby lymph nodes, you may receive chemotherapy and radiation therapy at the same time to shrink tumors prior to surgery.
At the highest stage, stage 4, the cancer has spread to other parts of your body. Treatment usually involves chemotherapy, targeted therapies or immunotherapy, which activates your body’s immune system to fight cancer. In advanced stages, oncologists may sometimes recommend radiation therapy to relieve pain and other symptoms.
If you or a loved one has received a colorectal cancer diagnosis, learn more about who is on the multi-disciplinary team and then request a consultation with one of our colorectal cancer specialists throughout Colorado.